Department of Medicine News
 Building Bridges at Med/Peds
Building Bridges at Med/Peds
Residents and attending physicians in combined Internal Medicine/Pediatrics, better known as "Med/Peds," often cross bridges in their daily work. They are used to moving amongst different age groups and their needs. Taking care of patients from diverse backgrounds in hospital and ambulatory settings frequently involves crossing cultural bridges. Over the past year, Med/Peds faculty and residents have been exploring some new bridges.
Dr. Suzanne McLaughlin, Med/Peds Residency Program and Division Director, has been conducting a monthly "Transition Clinic" which brings together skilled professionals from medicine, mental health, social work, and Rhode Island government agencies to help teens with chronic illnesses move from pediatric to adult-oriented care. During childhood, chronic conditions are treated within a pediatric model, which includes the family and a personal style of specialist care, using the pediatrician as communicator. Historically, since many of these patients weren't expected to survive into adulthood, pediatricians often continued to care for those with prolonged survival. However, with recent medical advances, more and more patients with chronic conditions are living well into adulthood and even going on to have their own children (who are sometimes affected by the same conditions). As patients reach more advanced ages, specialists trained to care for adults are often better prepared to provide them with age-appropriate specialty, preventive, and primary care.
Preparing teens and their families to move into the adult medical world can be a complex process. Chronic medical conditions can make the often-tumultuous adolescent years especially challenging for teens and families. As part of a healthy transition to adulthood, it is important for the teens who are capable of assuming their care to understand and take responsibility for their health issues, find suitable adult primary care and specialty providers, plan for post-high school education or work, navigate and secure government and local services, leave home, undertake financial planning as parents age, receive genetic counseling when appropriate, and address end of life issues, to mention a few common concerns. Med/Peds physicians are well suited to be the primary care physicians for these patients and can act as a stabilizing force for patients and families over the period of transition.
In Transition Clinic, Dr. McLaughlin and her team members have been working with patients and families to learn how to address these issues effectively. Nancy Bowering, RN, provides care coordination and nursing perspective, Jodie Senouillet brings a peer program for adolescents and young adults with chronic conditions, the RI Department of Health sponsors the involvement of an adult services specialist through the RIPIN program, and Dr. Richard Archambault works on the issues arising from transitions in family dynamics. Patients receive a comprehensive needs assessment, emergency and long-term care plans, and medical summaries. Many patients and families use the consult as a start-point for ongoing transition work with their primary and subspecialty providers. They can also receive assistance with needed referrals.
Looking back over the first year of sessions, Dr. McLaughlin notes, "It is definitely a learning process for us as well - the needs assessments uncover unique challenges for each patient and family, but provide an opportunity to learn from each patient and share the benefits with others. The key is having all of the information in one room and the knowledge of all the specialists who participate in clinic - this gives families a lot of options to develop the best transition plan for them."
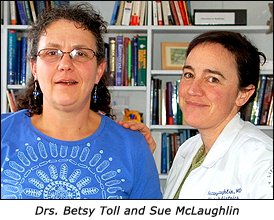
In a second bridge- building endeavor, Dr. Elizabeth Toll has been working to connect the worlds of primary care with those of mental health. As is typical of primary care physicians in general, Med/Peds doctors at RI Hospital encounter a high prevalence of common mental health problems like anxiety, depression, adjustment to major life changes, and posttraumatic stress disorder as well as the many barriers that prevent patients from reaching the mental health system. In response, Dr. Toll and psychiatrist-colleagues Michelle Rickerby, MD and Jody Underwood, MD have been conducting a study which aims address this ongoing dilemma. They are teaching a group of Med/Peds residents and attending physicians how to do basic mental health interventions in the primary care setting. These doctors are then implementing their new skills with a small number of patients. Both doctors and patients are study subjects. The study aims to look at the clinical efficacy and acceptability of this kind of treatment from the perspectives of both patients and doctors.
Study results are still pending, but informal feedback suggests that those involved have found the undertaking valuable. Doctors cite feeling more comfortable addressing mental health problems with all of their patients. They find the longer counseling visits a welcome counterpoint to typical busy internal medicine visits. They also feel they are able to demystify what goes on in mental health care and to make it more acceptable to patients who may need referral. They have become more comfortable communicating with mental health providers. Patients seem pleased to be able to receive care for emotional problems from the doctor who already knows them well and find the visits therapeutic. The Med/Peds study subjects have enjoyed collaborating with RIH psychiatrists. "We hope the study will help participants feel more comfortable integrating primary care and mental health care, an important concept of the medical home. We also believe this kind of work strengthens some of the skills that have always belonged to primary care physicians - forging strong doctor-patient relationships, listening actively, and understanding patients as people beyond their medical concerns," says Dr. Toll.

